What should the nurse practitioner’s “scope of practice” be and how autonomously should she or he be allowed to practice within that scope? A half century after the first advanced training programs brought nurses into the ranks of clinical providers, these two questions continue to bedevil nursing, medicine, insurance companies, and state legislatures. The crucial role of nurse practitioners in modern health care delivery, their ability to provide primary care, and the satisfaction of patients who receive this care – these facts are well-established and, for me at least, beyond dispute.
But questions of scope of practice and practice prerogatives (including prescribing privileges) remain contentious, and different state legislatures have codified different answers. I have no desire to enter debates that will likely continue at medical, nursing, and legislative levels for some time to come. But let me offer one historian’s perspective on a few aspects of these knotty issues.
The expansion of nursing’s role in the direction of specialized clinical expertise occurred in an amazingly brief stretch of time. In 1955, The American Nurses Association (ANA) approved a legal definition of nursing practice that prohibited “acts of diagnosis and prescription of therapeutic or corrective measures,” and it was only seven years later, in 1962, that it held its first clinical sessions at its annual convention.[1] Even then, until 1968, the ANA’s Code for Professional Nurses framed the nurse’s professional responsibilities in terms of the nurse’s relationship to physicians.[2] Yet, by the mid-60s, spearheaded by reforms in nursing education then underway, the term “nurse practitioner” came into use. It conveyed a nurse with “specialized expertise,” often in hospital settings, that grew out of additional training beyond the three years of hospital-based training that led to state licensure as a Registered Nurse.
“Specialized expertise” is an evocative but imprecise term. In nursing, it initially conveyed expertise in one or another aspect of hospital-based care. In the early 1900s, nurses acquired expertise as x-ray technicians and microscopists, and then again in the 1930s, they “specialized” in monitoring polio patients in their iron lungs. During World War II, nurses both on the front lines and in stateside hospitals began to perform venipunctures to administer fluids intravenously; after the war, they continued to do so, and some became specialized IV therapists, performing and monitoring IVs all along their units.
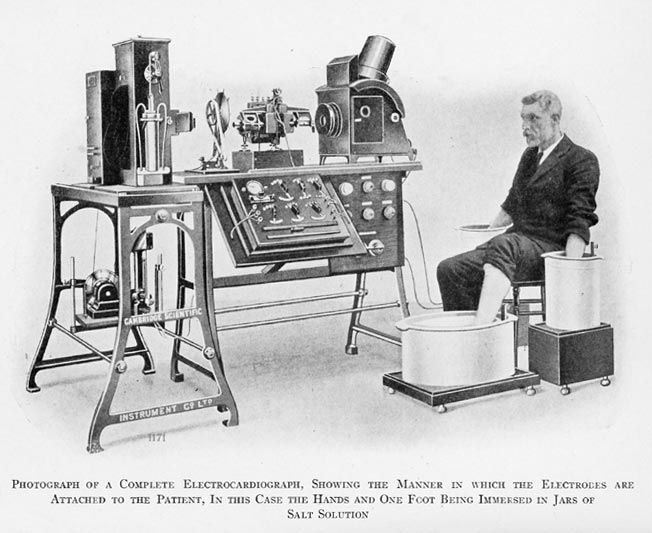
But in postwar America it was especially the new technologies brought to bear in treating acutely ill patients that elicited nurse specialization. Self-evidently, we needed critical care nurses, obstetrical nurses, and dialysis nurses able to exercise independent judgment and initiate (or discontinue) treatments in exigent circumstances, in what the historian Margaret Sandelowski terms “emergent life-threatening conditions.” By the 1960s, as Sandelowski observes, the new “machinery of care” had fostered a more collegial and collaborative relationship between physicians and nurses.[3] But this machinery – vital function monitors, cardiac monitors, electronic fetal monitors, and the like – was integral to medical care in the hospital. These monitors were not invented by nursing scientists as extensions of nursing care; they were instruments of improved hospital care whose design, manufacture, and intended use fell within the domain of physicians and the medical model.
The nomenclatural challenge proved even greater when advanced nursing practice left the hospital setting and became office-based, especially in the realm of primary care. Historians of nursing such as Julie Fairman tend to collapse the distinction between hospital-based specialty nursing and independent “nursing practice” in a global narrative of nursing’s coming-of-age in the four decades following the end of World War II. The storyline of professional self-becoming involves new forms of collegial collaboration between individual nurses and physicians, which, over time, empowered the nursing profession to liberate itself from the bondage of organized medicine, with its long-held belief in the subordinate role of nurses as physician extenders. What tends to be glossed over is the phenomenology of “expertise” in relation to different professional activities. Expertise in the implementation of technologically driven, hospital-based monitoring – with the diagnostic and treatment prerogatives associated with it – is not the same as the expertise that inheres in being a “practitioner” of medicine.
Or is it the expertise that inheres in being a “practitioner” of nursing? In her illuminating history of the nurse practitioner movement in America, Fairman delineates the inter-professional tensions congealed in this question. Even Loretta Ford and Henry Silver, she points out, who collaboratively developed the first (pediatric) nurse practitioner training program at the University of Colorado in the mid-1960s, used different, politically laden terminology to describe exactly what kind of nonmedical practitioner they were training. For the pediatrician Silver, the new provider would be a “nurse associate”; for the nurse educator Ford, she or he would be a “nurse practitioner.”[4]
And the linguistic-cum-political tension was played out in different pairs of descriptors. Nurse practitioners saw themselves as “taking on” diagnostic and treatment activities traditionally reserved for physicians, whereas physicians saw themselves as “delegating” certain medical tasks to nurses.[5] The need to define the nurse specialist’s prerogative to diagnose and treat illness as something other than “medical” was at the heart of the American Nurses Association’s need to distance itself from another nonmedically trained practitioner who emerged at this same moment in American history: the Physician Assistant. PAs were precisely what newly empowered clinical care nurses, at least in the eyes of their professional organization, did not want to be: a Physician Assistant rather than an autonomous Nurse Practitioner.[6]
In the realm of independent practice, this claim is highly problematic, since diagnosis and treatment of illness is not nursing “practice” in any historically meaningful sense of the term; rather, diagnosis and treatment have always fallen to the physician, as the word “physician” has been understood since the beginning of the thirteenth century, when Anglo-Normans gathered the Latin “physicus” and the French “physic” into the English “physic,” from which the word “physician” as a medical practitioner came in to use later in the century. It is easy to see how nursing practice can envelop sophisticated technological skills that are teachable and learnable. But the art of diagnosis and treatment – and the qualities of learned judgment[7] that fall to this task – have always been the province of medicine.
The historical claim enfolds an epistemic claim, a claim about the nature of different kinds of knowledge. Nursing knowledge, as codified in Florence Nightingale’s Notes on Nursing: What It Is and What It is Not (1859) and the British and American training programs that adopted her model in the 1870s and thereafter, has never been coextensive with medical knowledge. For Nightingale and her cohort of nursing educators, it remained a “gendered” (read: womanly) knowledge of comfort care; such care drew on sanitary science and scientifically informed bedside observation, both infused with a maternalistic sensibility.[8] Whether or not the knowledge base that subtends such patient-centered caring is something other than medical knowledge (as Nightingale believed) or a neglected subset of medical knowledge, is beside the point. And the point is this: The kind of “knowledge and skills”[9] that enter into independent clinical practice – “knowledge and skills” that, to be sure, nurse practitioners and other nonmedical providers can acquire to some extent – are by their nature medical. This is why the struggle of nurse practitioners to obtain state licensure that permits them to “practice” without medical supervision has been halting and may never succeed entirely.
It is not simply a matter of power in the sense of Foucault, of organized medicine’s ability to withhold, control, and/or regulate entry into the world of practice. It is because the science of clinical evaluation, diagnosis, and treatment that emerged in postbellum America was vested in the medical profession, not in the nascent nursing profession. In the final three decades of the nineteenth century, we behold the paradigm shift in medicine that historians endlessly write about: Medicine became scientific medicine, and this shift, with its associated educational and organizational changes, coincided with the emergence of a “profession” in the modern sense of the term. The physician, not his (then) helpmate nurse, was part of the profession vested with the scientific understanding of illness and the cultural authorization to act on this understanding by diagnosing and treating it.[10]
The foregoing helps explain why, in retrospect, the ANA’s insistence that pediatric nurse practitioners retain the prerogative to delineate their own scope of practice was foredoomed. ANA leaders sought to contest a notion of “practice” that, by the early 1970s, was incontestable. And the pediatric nurse practitioners knew as much. Like their nurse anesthetist forebears, who formed the National Association of Nurse Anesthetists in 1932,[11] they walked away from the ANA and formed their own professional association, the National Association of Pediatric Nurse Associates and Practitioners (NAPNAP) in 1973. And the NAPNAP, without further ado, accepted affiliation with the American Academy of Pediatrics, realizing that the ANA’s insistence on complete autonomy for nursing was self-defeating. The pediatric nurses, if not the ANA leaders, realized that such insistence militated against the idea of team practice, of a pediatrician, pediatric nurse practitioner, and nurse working together, and it contravened the reality that, in all such cases, the pediatrician would be the leader of the team.[12]
The dilemma for nurse practitioners is that they have spent over a half century trying to define themselves by what they are not. They are not physicians. They are not physician assistants or associates. They are not general nurses who lack advanced postgraduate training and specialty licensure. So what exactly are they?
In the late 1950s and 1960s, nurse educators like Esther Brown and Hildegard Peplau sought to fill in the lacuna by articulating a new basis for nurse practitioner expertise. In so doing, they adopted the same orientation as the founders of the “family practice” specialty movement during the same time. That is, they sought to equate the nurse practitioner’s “expert clinical practice” with a psychosocial sensibility and an ability to provide holistic psychotherapeutic care. Social science course work and psychodynamic training, they hoped, would move the nursing practitioner away from medicine and toward this new kind of nursing expertise.
That Brown and Peplau spearheaded this effort in nurse education is hardly surprising, given their respective backgrounds. Brown, a social anthropologist on the staff of the Russell Sage Foundation, authored Nursing for the Future (1948), a Foundation report that advocated university-based nurse training schools in the service of a vague psychosocial vision of nursing care. The nurse of the future, she wrote, would “complement the patient by supplying what he needs in knowledge, will, or strength to perform his daily activities and also to carry out the treatment prescribed for him by the physician.” Peplau, the founder of psychiatric nursing, followed an M.A. at Columbia’s Teachers College, where she completed the first course in advanced psychiatric nursing, with psychoanalytic training at New York’s William Alanson White Institute.[13] She believed that psychiatric nurses should function as psychotherapists, and, implicitly, that all nurses should bring a broad psychosocial, really a psychotherapeutic, orientation to their work. Were Brown, Peplau, and their associates successful in reforming nursing training in a manner that subserved a new kind of nursing identity? No, certainly not in the manner they envisioned. And further, at the time their educational reforms were introduced in the nursing schools of large public universities, there were serious problems: Graduates overfed with the new social science curriculum were simply unprepared to assume the responsibilities of nursing practice.[14]
_______________________
My father, William Stepansky, whose remarkable postwar career in family medicine has been woven into many of these essays, was a pharmacist before he was a physician. He entered Philadelphia College of Pharmacy and Science in 1940, but his education was interrupted by induction into the army in March, 1943, several months before he completed his junior year. He had not begun pharmacy college with the intention of attending medical school – this seemed an utterly far-fetched dream for the son of poor Russian émigrés who fled the Pogroms in 1921 and struggled to raise a family in the Jewish enclave of South Philadelphia. His own mother thought him foolish for entering college and crazy (meshuga) when he mentioned his interest in medicine. In 1946, after two years of service as a surgical technician on the battlefields of France, Belgium and Germany and an additional six months as a laboratory technician in Pilzen, Czechoslovakia, he returned to Philadelphia, where he completed his pharmacy training in 1947. Only then, with the G.I. Bill in place, did he allow himself to envision a career in medicine, and following an inventive series of initiatives, he gained admittance to Jefferson Medical College, where he joined the freshman class in the fall of 1948.[15]
My father not only retained an active pharmacy license throughout his career, but actually “practiced” pharmacy out of his Trappe office. He maintained an impressive inventory of basic and not-so-basic drugs, and he concocted, among other things, the marvelous “red medicine” of which I have written. He became a staff research clinician for McNeil Labs and later participated in clinical drug trials with the Psychopharmacology Research Unit of the University of Pennsylvania. Pharmacy training certainly proved helpful to him and his rural patients, but it was not at the core of his professional identity. He was not a “pharmacist practitioner” or an “advanced practice pharmacist.” He was a physician, a general practitioner of medicine.
Perhaps it is time for the nurse practitioner profession to dispense with the “nurse” appellation altogether. These men and women are not professional nurses as the notion of nurse professionalism took shape over 150 years, even though they come to medical “practice” through nursing training and the patient-centered values it instills. But additional clinical training of several years duration beyond the R.N. or B.S.N. level, I suggest, takes them out of the realm of nursing practice altogether. So, with a nod to perduring intra- and inter-professional politics, let’s cast aside the terms “medical,” “physician,” “nurse,” and “nursing” altogether, and come up with something more accurate. Advanced practice nurses should henceforth be designated “licensed clinical providers” or “licensed clinical practitioners,” with the appropriate specialty designation appended to their licenses, e.g., “licensed clinical provider – primary care” or “licensed clinical provider – nephrology” or “licensed clinical provider – oncology.” There, I’ve said it. These designations are accurate and neutral and therefore certain to please no one.
__________________
[1] J. Fairman, Making Room in the Clinic: Nurse Practitioners and the Evolution of Modern Health Care (New Brunswick: Rutgers University Press, 2008), pp. 119-21.
[2] L. Freitas, “Historical roots and future perspectives related to nursing ethics,” J. Prof. Nurs., 197-205, 1990, at 202.
[3] M. Sandelowski, Devices and Desires: Gender, Technology, and American Nursing (Chapel Hill: University of North Carolina Press, 2000), pp. 127-28.
[4] Fairman, Making Room in the Clinic, p. 91.
[5] J. Fairman, “Delegated by default or negotiated by need?: physicians, nurse practitioners, and the process of clinical thinking,” in E. D. Baer, et al., Enduring Issues in American Nursing (NY: Springer Pub., 2002), pp. 309-333, at p. 323.
[6] Fairman, Making Room in the Clinic, pp. 95ff.
[7] N.B. I do not understand “clinical judgment,” with its reliance on mentoring and tacit knowing, in the same way Fairman understands “clinical thinking,” viz., as a process or skill set. See Fairman, “Delegated by default,” pp. 311-12 and Making Room in the Clinic, p. 187.
[8] For a wonderful popular exposition of Nightingale’s vision of the nurse transposed to the Bellevue Hospital Training School in the early 1880s, see F. H. North, “A new profession for women,” The Century, 25:30-37, 1882.
[9] Fairman, “Delegated by default,” p. 323.
[10] These brief remarks allude to, without doing justice to, the brilliant analysis of Thomas Haskell on the emergence of modern professions in postbellum America. See T. L. Haskell, The Emergence of Professional Social Science: The American Social Science Association the the Nineteenth-Century Crisis of Authority (Baltimore: John Hopkins, 2000 [1977]), pp. 68-74, 91-121, and passim.
[11] K. Koch, “Agatha Hodgins, Lakeside Alumnae Association, and the founding of the AANA,” AANA Journal, 73:259-62, 2005.
[12] Fairman, Making Room in the Clinic, pp. 175-80.
[13] On Peplau’s graduate training at Teacher’s College and the William Alanson White Institute, see B. J. Callaway, Hildegard Peplau: Psychiatric Nurse of the Century (NY: Springer Pub., 2002), pp. 167-91.
[14] Dominique Tobbell documents the perceived deficiencies of 1960s graduates of the UCLA and University of Minnesota nursing schools, where the new curriculum was implemented, in “’Coming to grips with the nursing question’: the politics of nursing education reform in 1960s America,” Nurs. Hist. Rev., 22:37-60, 2014.
[15] This paragraph is culled from my memoir of my father’s life and career, P. E. Stepansky, The Last Family Doctor: Remembering My Father’s Medicine (Montclair, NJ: Keynote, 2011).
Copyright © 2014 by Paul E. Stepansky. All rights reserved.