“Mustard gas burns. Terrific suffering.”
[The fourth of a series of essays about the gallant nurses of World War I commemorating the centennial of America’s entry into the war on April 6, 1917. The nursing care of soldiers exposed to poison gas on the Western Front is explored at greater length in chapter 4 of Easing Pain on the Western Front: American Nurses of the Great War and the Birth of Modern Nursing Practice (McFarland, 2020)].
Now, sadly, chemical weapons are back in the news. But large-scale chemical warfare reaches back over a century. In WWI, Germany released 5,730 cylinders of chlorine gas across a four-mile stretch of no-man’s-land into the Allied lines during the Second Battle of Ypres in April, 1915. Thus the birth of chemical warfare. Britain replied in kind, releasing cylinders of chlorine gas during the Battle of Loos the following summer, and Germany upped the horror in July, 1917, delivering artillery shells filled with dichlor-ethyl-sulphide or “mustard gas” just prior to the Third Battle of Ypres.
Chlorine gas attacked the airways. Severe respiratory swelling and inflammation killed many instantly and the rest struggled to nearby casualty clearing stations with acute congestion of the lungs, pneumonia, and blindness. Soldiers who had inhaled the most gas arrived with heavy discharge of a frothy yellow fluid from their noses and mouths as they drowned in their own secretions. For the rest, partial suffocation persisted for days, and long-term survivors had permanent lung damage, chronic bronchitis, and occasionally heart failure. Mustard gas burned the skin and respiratory tract, stripping the mucous membrane off the bronchial tubes and causing violent inflammation of the eyes. Victims were left in excruciating pain and utterly helpless.[1]
Nurses, no less than physicians, were initially confused about the nature of the gas and the severity of its effects.[2] But they quickly came up to speed and realized that soldiers suffering from poison gas posed a nursing challenge no less formidable than those dying from gangrenous wounds. Nurses were accustomed to losing patients, but not to being powerless to provide comfort care, to ease patients’ agony during their final days. How to nurse on when nursing was unavailing, when the burns were so terrible that “nothing seems to give relief”?[3]

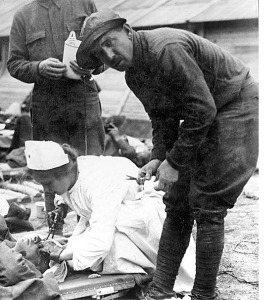
WWI nurses in gas masks treat soldiers after a gas attack
Of course, nurses did what little they could. Inflamed eyes were repeatedly irrigated with alkaline solution. Respirators soaked in hyposulphate could be provided to patients able to use them. At American Base Hospital 32, soldiers who had breathed in mustard gas were given a mixture of guiacol, camphor, menthol, oil of thyme, and eucalyptus that caused them to expectorate inflammatory material. According to Maude Essig, an American Red Cross Nurse who worked at the hospital, the nurses helped devise it.[4]
According to Essig, the mixture provided some temporary relief to soldiers with burning throats and mouths. But nurses otherwise echoed a shared sense of impotence when it came to making gassed patients comfortable. During the Second Battle of Ypres, when chlorine gas was first used by the Germans, Canadian nurse Agnes Warner recalled the initial wave of gassed troops: “There they lay, fully sensible, choking, suffocating, dying in horrible agonies. We did what we could, but the best treatment for such cases had yet to be discovered, and we felt almost powerless.”[5] Shirley Millard was graphic in describing the severe burn patients who rendered nursing futile. “Gas cases are terrible,” she wrote at war’s end in November, 1918.
They cannot breathe lying down or sitting up. They just struggle for breath, but nothing can be done . . . their lungs are gone . . . literally burnt out. Some with their eyes and faces entirely eaten away by the gas, and bodies covered with first degree burns. We try to relieve them by pouring oil on them. They cannot be bandaged or even touched.[6]
Whereas soldiers with even the worst of battlefield wounds usually did not complain, the gas cases “invariably are beyond endurance and they cannot help crying out.” Millard’s judgment was affirmed by many others. Maude Essig wrote of a “star patient,” one Leo Moquinn, who “was terribly burned with mustard gas while carrying a pal of his three-quarters of a mile to safety after the gas attack. Except for his back, she added, his “entire body is one third-degree burn. He cannot see and has developed pneumonia and he is delirious.”[7] Such were the burn patients.
Essig’s reference to pneumonia alludes to the multitude of infectious diseases that accompanied battlefield wounds and complicated (or prevented) recovery. Pneumonia could be rampant during winter months; gangrene and tetanus were prevalent year round. Typhoid was partially controlled by the antityphoid serum injections troops received, usually prior to disembarkation but otherwise in the reception huts of clearing stations and field hospitals. But bronchitis, trench fever, diphtheria, cholera, dysentery, meningitis, measles, mumps, erysipelas,[8] and, finally, influenza, were not. Nurses recorded deaths resulting from various combinations of the foregoing, such as Edith Appleton’s “poor little boy, Kerr,” who died of gas, pneumonia, and bronchitis.[9]
Infected shrapnel and gunshot wounds could be irrigated or bathed continuously in antiseptics, first developed in the 1870s and packed in sterile dressings available in sealed paper packages since 1893.[10] But in the preantibiotic era, nursing care of systemic infections was limited to the same palliatives we employ today: rest, warmth, hydration, nutrition, aspirin (and, back then, quinine), all amplified by the nurse’s caring, maternal presence.
Trench foot, a combination of fungal infection, frostbite, and poor circulation, was endemic during the winter months, when soldiers lived in trenches flooded with icy water, often waist-high, for days on end. They struggled into clearing stations with feet that were “hideously swollen and purple,” feet “that were “raw with broken blisters and were wrapped in muddy, dripping bandages.”[11] But trench feet, however disabling, at least permitted more active measures. In addition to giving morphine, there was a treatment protocol to follow, such as this one at a British Military Hospital in the winter of 1917:
We had to rub their feet every morning and every evening with warm olive oil for about a quarter of an hour or so, massage it well in and wrap their feet in cotton wool and oiled silk – all sorts of things just to keep them warm – and then we put big fisherman’s socks on them. Their feet were absolutely white, swollen up and dead. Some of their toes dropped off with it, and their feet looked dreadful. We would say, ‘I’ll stick a pin in you. Can you feel it?” Whenever they did feel the pin-prick we knew that life was coming back, and then we’d see a little bit of pink come up and everybody in the ward would cheer.”[12]
It is the dizzying confluence of multiple battlefield injuries, many gangrenous, with the effects of poison gas and intercurrent infectious diseases that threatened to, and occasionally did, overwhelm the WWI nurses. Reading their diaries and memoirs, one sees time and again how the nurses’ calling, amplified by the camaraderie of other nurses, surgeons, and orderlies who felt similarly called, overpowered resignation and despair. In a diary entry of September 14, 1916, Kate Luard referred to the “very special nursing” required by soldiers with multiple severe injuries. She had in mind
The man with two broken arms has also a wound in the knee – joint in a splint – and has had his left eye removed today. He is nearly crazy. Another man has compound fractures of both legs, one arm, and head, and is quite sensible. Another has both legs amputated, and a compound fracture of [the] arm. These people – as you may imagine – need very special nursing.[13]
If one adds to such clusters the serious general infections that often accompanied battlefield injuries, one has some sense of what nurses were up against, and just how special their nursing had to be. When influenza, the deadly Spanish flu, began to swamp clearing stations and hospitals in the spring of 1918, nurses simply added it to the list of challenges to be met with the resources at hand. And they did so in the knowledge that as many as half of the infected would die.[14] Beatrice Hopkinson, a British auxiliary nurse, recorded the new protocol developed at her General Hospital in St. Omer to meet the rush of influenza patients:
During those early days of the flu the treatment was to strip the patients in one tent, their clothing going immediately to the fumigator. Then, the patient was bathed in disinfectant and taken to the different wards. Some of the patients were very ill and died with pneumonia after a few days.[15]
The early days of the pandemic gave way to the later days, and after the Armistice was signed on November 11, 1918, nurses occasionally felt boredom, even mild malaise, when the demands of “special nursing” relented and they increasingly found themselves nursing “mostly mild influenza cases.”[16]
I admire the nurses of WWI because they did what was required of them absent any preexisting sense of what they could be required to do, absent, that is, anything approaching a “job description.” Without medical residents, internists, and infectious disease specialists to fall back on, they collapsed specialism into global care-giving identities. This meant they managed multiple war wounds and intercurrent infections, prioritizing among them and continuously adjusting treatment goals in the manner of highly skilled primary care physicians. By the same token, they realized the importance of compassion in the face of ameliorative impotence. Somehow they found time to be present, to slip into a ward with a soldier dying of gas gangrene every few minutes “to do something perfectly useless that might perhaps give a ray of comfort.”[17]
Ironically, given the environment in which they labored and their “patient population” of soldiers in extremis, the nurses embodied the values of primary care medicine, since they took upon themselves the role of primary caregivers obligated to stay with their patients through thick and thin, to summon senior colleagues and surgeons as needed, and to ease life transitions, whether to recovery, convalescence, lifelong disability, or death.[18] And they did so whatever the weight of multiple assaults on their own bodily and mental integrity.
Nurses, technically noncombatants, suffered alongside the troops. During rushes, their clearing stations, hospitals, and living quarters were under land and air assault and occasionally took direct hits. They contracted infectious diseases, especially flu,[19] during which they usually carried on with the aid of simple analgesics until they felt better or worse. When Helen Boylston became feverish in November, 1918, a symptom she attributed to diphtheria, she braced herself for a long-awaited evening dance with “quantities of quinine and finally a stiff dose of whiskey, and I felt ready for anything.” But not ready enough, it turned out. She collapsed at the dance with a bad chill and had to be carried to her bed. When she went on duty the following day, she became delirious in the ward and was lugged off by an orderly and subsequently seen by a doctor. “So here I am,” she wrote in her diary. “I’ve developed a heart and a liver, and am as yellow as a cow-lily. I have to lie flat on my back and be fed. For three days I lay motionless all day long, not caring to move or to speak, I was so tired.” Boylston was soon joined by a second nurse with diphtheria, placing the camp “in a panic,” with every staff member now given daily throat cultures.[20]
Despite training in the use of gas masks in the event of direct shelling, mask-less nurses suffered the effects of poison gas from daily proximity to patients on whom the shells had landed. Their own vulnerability to gas attack and attenuated exposure to the poison lent special intensity to their care of burn victims. They understood, with Maude Essig, that mustard gas burns indeed meant “terrific suffering.”[21] Whether infected or poisoned, they usually labored on until they collapsed or were so near collapse that medical colleagues ordered them out of the wards, whether to bed, to a general hospital for treatment, or to a nearby convalescent homes for recuperation and a desperately needed “time out.”[22]
Civil War nurses too eased transitions to death, but their nursing goal during a soldier’s final days was to reconfigure mortal battlefield injury into the promise of a beneficent afterlife. So they stayed with the dying, soliciting final confessions of sinful living, allowing soldiers to reminisce and reflect, and soliciting (and writing down) words of comfort to sustain family members in believing that their soldier had died a “good death.”[23] World War II, on the other hand, witnessed the development of new vaccines, a national blood bank program, the widespread availability of sulfa drugs in 1941 and penicillin in 1944, major advances in the control of shock and bleeding and in battlefield surgery, and much greater speed of evacuation of the seriously wounded to European and stateside base hospitals. Taken together these advances created a buffer between nurses and the prolonged witnessing of soldiers dying in unrelievable pain.
It was the nurses of WWI who took it on the chin. They could not sustain themselves and their patients with the naturalistic view of the afterlife popular during the Civil War.[24] Nor did they have the benefit of more “modern” technology and organization to shield them, if only somewhat, from the experiential onslaught of dying soldiers. It was not death per se but the agony of dying – from infected battle wounds and/or systemic infections, gas gangrene, chlorine and mustard gas, rushed amputations followed by reinfection and blood loss – that took them to their own existential no-man’s-land, the kind we encounter in the writings of Mary Borden and Ellen LaMotte.
In the summer of 1917, the nurses at No. 12 General Hospital on the outskirts of Rouen struggled with a gas victim whose paroxysms of coughing came every minute and a half “by the clock,” and who had not slept in four days. To quiet him, they rigged up a croup tent under which they took turns holding a small stove that heated a croup kettle from which the soldier could breathe the steam. When sleep finally came, they were “ready to get down on their knees in gratitude, his anguish had been so terrible to watch.” To their head nurse, Julia Stimson, they remarked that “they could not wish the Germans any greater unhappiness than to have them have to witness the sufferings of a man like that and know that they had been the cause of it.”[25]
It was bearing witness to unrelievable suffering that was the worst assault borne by the nurses. “It is dreadful to be impotent, to stand by grievously stricken men it is impossible to help, to see the death-sweat gathering on young faces, to have no means of easing their last moments. This is the nearest to Hell I have yet been.” This is the voice of an anonymous British Red Cross nurse, unsettled by the dying Belgium soldiers she encountered on ambulance runs in the fields of West Flanders in the winter of 1915. The American nurses at No. 12 General Hospital brushed up against this same hell, and they could think of no greater punishment for enemy combatants than to witness what they witnessed, often for weeks on end. And yet the nurses of WWI were not stymied by seeming impotence in the face of pain. They labored on to the breaking point in the service of soldiers who, all too often, were already broken. This makes them warriors of care and, in a devotion to patients that was literally and not metaphorically self-less, heroes of the first rank.
_______________________
[1] Christine E. Hallett, Veiled Warriors: Allied Nurses of the First World War (Oxford: OUP, 2014), 79-80, 203.
[2] E.g., Julia C. Stimson, Finding Themselves: The Letters of an American Army Chief Nurse in a British Hospital in France (NY: Macmillan, 1918), 80; John & Caroline Stevens, eds., Unknown Warriors: The Letters of Kate Luard, RRC and Bar, Nursing Sister in France 1914-1918 (Stroud: History Press, 2014), loc 1945.
[3] Maude Frances Essig, My Trip with Uncle Sam, 1917-1919: How We Won World War I, unpublished journal written during the summer, 1919, entry of March 24, 1918.
[4] Agnes Warner, My Beloved Poilus’ (St. John: Barnes, 1917), loc 861.
[5] Warner, My Beloved Poilus’ , loc 814.
[6] Shirley Millard, I Saw Them Die: Diary and Recollections (New Orleans, LA: Quid Pro, 2011), loc 514.
[7] Essig, My Trip with Uncle Sam, entry of March 24, 1918.
[8] Erysipelas is an acute bacterial infection of the upper dermis, usually of the arms, legs, and/or face, that is accompanied by red swollen rashes. Without antibiotic treatment, It can spread through the blood stream and cause sepsis.
[9] Edith Appleton, A Nurse at the Front: The First World War Diaries, ed. R. Cowen (London: Simon & Schuster UK, 2012), 111.
[10] Rodney D. Sinclair & Terence J. Ryan, “A Great War for Antiseptics,” Australas. J. Dermatol, 34:115-118, 1993. These nineteenth-century antiseptics included salicylic, thymol, Eucalyptus oil, aluminum acetate, and boric acid.
[11] Helen Dore Boylston, Sister: The War Diary of a Nurse (NY: Ives Washburn, 1927), loc 154.
[12] Kathleen Yarwood (VAD, Dearnley Military Hospital), in Lyn MacDonald, The Roses of No Man’s Land (London: Penguin, 1993 [1980]), 197-198.
[13] Luard, Letters, loc 1245.
[14] Millard, I Saw Them Die, loc 472.
[15] Beatrice Hopkinson, Nursing through Shot & Shell: A Great War Nurse’s Story, ed. Vivien Newman (South Yorkshire: Pen & Sword, 2014), loc 1999.
[16] Hopkinson, Nursing Through Shot & Shell, loc 2609.
[17] [Kate Norman Derr] “Mademoiselle Miss”: Letters from an American Girl Serving with the Rank of Lieutenant in a French Army Hospital at the Front, preface by Richard C. Cabot (Boston: Butterfield, 1916), 76-77.
[18] For an exposition of these values and how they gained expression in American medicine in the nineteenth and twentieth centuries, extending through “general practice” of the 1950s and ’60s, see Paul E. Stepansky, In the Hands of Doctors: Touch and Trust in Medical Care (Santa Barbara: Praeger, 2016).
[19] “The flu is back again and everybody has it, including me. I’ve run a temperature of one hundred and two for three days, can hardly breathe, and have to sleep on four pillows at night.” Boylston, Sister, loc 630.
[20] Boylston, Sister, loc 1350, 1357.
[21] Essig, My Trip with Uncle Sam, entry of March 23, 1918.
[22] E.g., Luard, Letters, loc 1247: “Sister D, the Mother of all the Abdominals, has her marching orders and goes down to Rouen to a General Hospital tomorrow. Her loss is irreparable.” Edith Appleton recounts taking care of three sick nurses and a sick VAD at one time: “I have begun to feel like a perpetual night nurse to the sick sisters as I have another one to look after tonight with an abscess in her ear”(A Nurse at the Front, p. 123). Maude Essig contracted erysipelas in the spring of 1918 and reported feeling “awfully sick” the following fall, when she relied on “quinine and aspirin in large doses” to keep going (My Trip with Uncle Sam, entries of April 9, 1918, April 14, 1918, and October 27, 1918).
[23] Drew Gilpin Faust, This Republic of Suffering: Death and The American Civil War (New York: Vintage, 2008), chapter 1.
[24] Faust, Republic of Suffering, pp. 178, 187.
[25] Stimson, Finding Themselves, pp. 80-81.
Copyright © 2017 by Paul E. Stepansky. All rights reserved. The author kindly requests that educators using his blog essays in their courses and seminars let him know via info[at]keynote-books.com.