“He’s saved, and that makes up for much.”
[The third of a series of essays about the gallant nurses of World War I commemorating the centennial of America’s entry into the war on April 6, 1917. Learn more about the range of battlefield injuries and infectious diseases treated by nurses on the Western Front in Easing Pain on the Western Front: American Nurses of the Great War and the Birth of Modern Nursing Practice (McFarland, 2020)].
Of course the surgeons of WWI could only save so many lives. During battle “rushes,” when they operated up to 16 hours a day, they had to husband operative energy for soldiers who were savable, especially those whose saving could land them back in the trenches. Many cases were deemed hopeless and simply handed back to the Sisters, to provide what meager palliative care they could while the soldiers awaited death in the tent set aside for them, the Moribund Ward. But the Sisters sometimes refused to let matters rest, recognizing that the surgeons, often operating at breakneck speed in a state of exhaustion, did not have the last word on life and death. So soldiers out of surgeons’ hands might still find themselves in nurses’ hands, where they were beneficiaries of nursing so intensive and prolonged that, against all odds, it segued into a curative regimen.
Mary Norman Derr, an American nurse trained by the French Red Cross in 1914 and assigned to a French Army Hospital near the trenches of the Marne in 1915, recalled an Arab soldier who arrived at the hospital barely conscious. His seven suppurating wounds led to two successive operations, after which surgeons pronounced him hopeless and handed him back to Nurse Derr:
It is one of the few dressings I have had that really frightened me; for it was so long, and every day for a week or more, I extracted bits of cloth and fragments of metal, sometimes at a terrifying depth. Besides my patient was savage and sullen, all that is ominous in the Arab nature. Gradually, however, the suppuration ceased, the fever fell, and suddenly one day Croya smiled.[1]
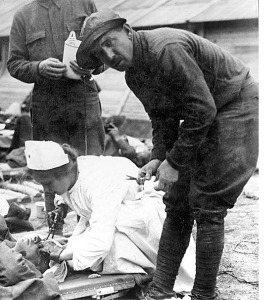
An American Red Cross nurse at work outside a French field hospital, 1915
MGH-trained Helen Dore Boylston, working in the post-surgical bone ward of her Base Hospital in the winter of 1918, was no stranger to surgical aftercare. Boylston enjoyed her 40 patients, and singled out a pluck Australian of over sixty with a leg “torn to pieces.” “He’s a Crotchety old darling, always raging and roaring about something,” she wrote her family:
One day, when I was here before, he complained of a pain in his thigh and began to run quite a temp. As his leg was laid wide open anyhow, I took a look along the bone, Dad meantime cursing the roof off. I found a walled-in pus pocket, and picking up a scalpel told Dad he’d better look out of the window for a minute, as I was going to have to hurt him. Then, before he knew what I was about, I had slit the thing open. At least two cupfuls of pus poured out, and his relief was tremendous at once. Of course his temp dropped, too. I put in a packing and watched it for a few days. It cleared up promptly. That was absolutely all.”[2]
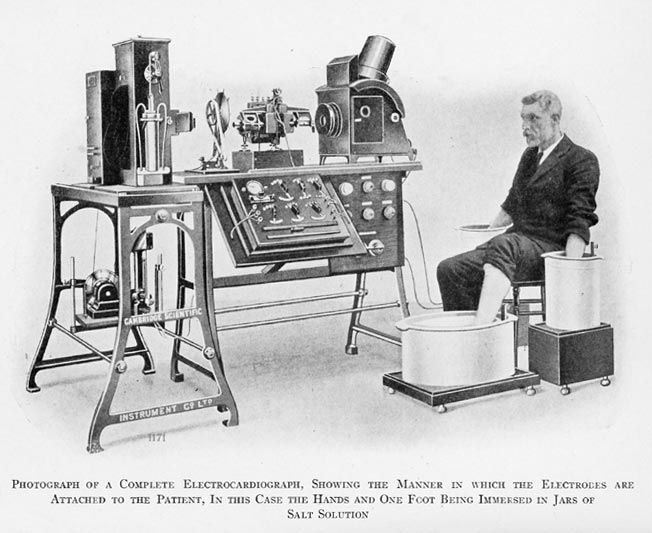
Nor did interventionist nursing end with bedside surgery. Nurses often believed rehabilitation was possible when doctors did not, and they proved their point with paralyzed soldiers who, so the surgeons declared, would never walk again. Consider Agnes Warner, a Canadian nurse working at the American Hospital in Neuilly, France. Casualties from Alsace poured into the hospital in the spring of 1915, at which time a surgeon remarked that one of her patients, her “poor paralyzed man,” would never walk again. Unfazed by the pronouncement and unwilling to rest content giving the patient English lessons to help pass the time, she devised a program of rehabilitation that incorporated electrical stimulation, which only became available at the Hospital in late June. Three weeks later, she had her paralyzed man out on the balcony, where he enjoyed fresh air for the first time in six months. She was assigned another patient paralyzed from the waist down a month later, and then in mid July she proudly reported on both patients:
My paralyzed man stood up alone last Sunday for the first time and now he walks, pushing a chair before him like a baby. He is the happiest thing you can imagine; for seven months he has had no hope of ever walking again. . . . My prize patient, Daillet walks down stairs by himself now . . .We are all proud of him. The doctor who sent him here from Besancon came in the other day to see how he was getting on and he could not believe it when he saw him.[3]
Worst of all were soldiers whose gaping wounds and limbless stumps were saturated with anaerobic bacteria of the genus Clostridium– soil-dwelling bacteria that thrive in the absence of oxygen – from the heavily fertilized fields of Flanders and Northern France. The bacteria entered cavities through dirt and debris picked up by exploding shell fragments; bullet wounds and shrapnel typically drove into the body with pieces of bacteria-infested clothing. The result was the dreaded gas gangrene, easily detected by the darkened muscle, bubbling sound, and overpowering stench[4] emanating from the infected limb or body cavity. Nurses could smell such cases a mile away (so to speak), and dreaded removing original aid station bandaging, often four or five days old, that revealed the “hideous and hopeless color of gangrene.”[5] Prompt treatment in a Casualty Clearing Station (CCS), which typically meant amputation of an infected limb and antiseptic irrigation, might save a soldier’s life. But left unattended in trenches and on battlefields for three, four, even five days, soldiers arrived at clearing stations with septicemia (blood poisoning), which foretold an agonizing death, often within hours, almost always within a few days.
Among the multitude of stressors that made up ward nursing in CCSs and field hospitals, ministering to dying gangrenous soldiers was at the top of the list. What is remarkable is that even here nurses occasionally rejected the medical verdict and resolved to nurse on with those awaiting death in the Moribund Ward. This was true of Kate Luard, who, in the midst of the Battle of Arras in May, 1917, battled on for her dying soldiers. She was, she wrote home, “engaged in a losing battle with gas gangrene again – in the Moribund Tent – a particularly fine man, too.” But then, a month later, she began working with “two given-up boys” who could not be revived the preceding day. Still, the boys seemed to her “not hopeless” and she resolved to “work” on them. The result repaid the effort, “and after more resuscitation they are now both comfortably bedded in one of the Acute Surgicals, each with a leg off and a fair chance of recovery.” A few days later, she wrote that her “two resuscitated boys in the Moribund Ward are all right.” To be sure, many dying soldiers were revived only to develop gangrene above their amputations and die, but Luard never stopped trying. If one of her gangrenous boys was “going wrong” on a particular day, she would counter that “moribund head cases are smoking pipes and eating eggs and bread and butter. The kidney man is being dressed with [the antiseptic] Flavine and has had a leg off and is nearly convalescent!”[6]
The vast majority of nursing saves went unrecorded, perhaps noticed at the time by a colleague, a supervisor, even the Head Matron. Without the wartime diaries and letters the nurses left behind, we would have little inkling of their quiet struggles to keep forsaken soldiers alive. Such struggles take us far from the world of high-tech nursing, even in its low-tech WWI incarnation. What we behold, rather, is hard-core, soft-touch nursing, abetted by a Rube Goldberg inventiveness in making use of materials at hand, somehow garnering materials not easily obtainable, and then patiently titrating treatments (including food intake) in a manner responsive to states of severe, even deathlike, debilitation.
A little Night Sister in the Medical last night pulled a man round who was at the point of death, in the most splendid way. He had bronchitis and acute Bright’s Disease, and Captain S. and the Day Sister had all but given him up; but at 10:30 p.m., as a last resource, Captain S. talked about a Vapour Bath [steaming up his room], and the little Sister got hold of a Primus [stove] and some tubing and a kettle and cradles, and got it going, and did it again later, and this morning the man was speaking and swallowing, and back to earth again. He is still alive tonight, but not much more.[7]
You will like to hear of the living skeleton with wounds in back and hands and shoulder that they brought me filthy and nearly dead from another pavilion. That was nine days ago. I diagnosed him as a case of neglect and slow starvation, and treated him accordingly – malted milk, eggs, soap, and alcohol to the fore. His dressing took one and a half hours every day, and all nourishment given a few drops at a time, and early all the time, for he was almost too weak to lift an eyelid, much less a finger. This morning he actually laughed with me and tried to clench his fist inside the dressings to show me how strong he was. He’s saved, and that makes up for much.[8]
I happened on a corpse-like child [a teenage soldier] the other day being brought into the Moribund Ward to die and we got to work on resuscitation, with some success. He had been bleeding from his subclavian artery and heard them leave him for dead in his shell-hole. But he crawled out and was eventually tended in a dug-out by ‘a lad what said prayers with me,’ and later the hole in his chest was plugged and he reached us – what was left o of him. When, after two days, he belonged to this world again, I got Capt. B. to see him, and he got Major C. to operate and tied the twisted artery which I had re-plugged – he couldn’t be touched before – and cover with muscle the hole through which he was breathing, and he is now a great hero known as ‘the Prince of Wales’.”[9]
Nor was orthopedic inventiveness beyond the pale. In fracture wards up and down the Front, war nurses were adepts of the Balkan frames affixed to beds, virtuoso adjusters of the heavy weights and cables that maintained constant traction of fractured long bones suspended from above. But they improvised as well. Kate Derr provides an example of the ingenious contraption rigged up by war nurses for a soldier with badly damaged joints. She wrote home from Vitry in April, 1917 of her “lastingly satisfactory” work on a soldier who had “double anthrotomie [deep lacerations] of the knees.” She explained that
when he came the insteps were bent like a ballet-dancer’s. Even admitting his recovery, which seemed impossible, he would be obliged to go about on the points of his toes, the knees being permanently stiff. At first, after ‘peeling’ with every conceivable dissolvent, I began just the slightest effleurissage [circular stroking] which developed into massage, and then I invented an apparatus . . . A board about 14 inches square was padded with cotton and swathed neatly in a bandage. This was laid vertical against the soles of the feet which I tried to place as nearly as possible in a normal position. Then I attached a bandage (having no elastic, which would have been better) to the head rail of the bed on one side, passed it around the board and up the other side, fastening it again to the rail as taut as possible. The knot was tightened twice a day. Result – in two weeks those refractory feet had regained a proper attitude.[10]
Such dedication to severely injured patients persisted in the face of bombings that reached and sometimes destroyed the clearing stations and field hospitals in which the nurses worked. Nurses too were casualties of war and disease. In Belgium in the fall of 1917, enemy bombs destroyed the 58th General Scottish Hospital adjacent to Beatrice Hopkinson’s own 59th. Hopkinson watched while orderlies from her hospital “stooped over bunches of twigs in various places and picked up something, putting it in the sheet. They were the arms and legs and other pieces of the patients that had been bombed and blown right out into the [outlying] park.”[11] Back in her own hospital, with bombs continuing to fall, she confided to her diary that “My knees just shook and, had I allowed it, my teeth would have rattled; but I had to be brave for my patients’ sake. When they saw the womenfolk apparently without fear it kept them brave.”[12]
Nurses like Hopkinson, Warner, Luard, and Derr did not see themselves as brave. Rather, their sense of duty was so powerful that it sequestered fear and compelled action in ways that would have been incomprehensible to their non-nursing selves. “I never realized what the word ‘duty’ meant until this War,” Hopkinson remarked. Hers was the courage of the Hippocratic caregiver, who subordinates self-interest to the patient’s well-being. For the nurses of WWI, such subordination extended to self-preservation itself. I admire them because their sense of mission remained unswerving as moribund wards swelled and they failed, time and again, to “pull round” those too far gone to be pulled. Living and working amid the bodies of those they failed to save – perhaps because they lived and worked among those they failed – the nurses remained certain of who they were and what they did. They were vindicated by their calling. Thus Kate Luard during the Battle of Arras in the fall of 1916:
There is no form of horror imaginable, on any part of the human body, that we can’t tackle ourselves now, and no extreme of shock or collapse is considered too hopeless to cope with, except the few who die in a few minutes after admission.[13]
And with the resolve to nurse on, even during bombing raids that imperiled them, came defiant resiliency. The clearing stations right off the Front were, in the words of the American nurse and poet Mary Borden, the second battlefield – a battlefield littered with care giving paraphernalia that combatted and succumbed to the inexorability of death. So why did the nurses labor on? “He’s saved, and that makes up for much,” declaimed Kate Derr in the fall of 1915. To which Kate Luard added her own gloss a year and a half later:
Some of us and Capt. B. have been having a bad fit of pessimism over them all lately, wondering what is the good of operations, nursing, rescues, or anything, when so many have died in the end. But even a few miraculous recoveries buck one up to begin again.[14]
____________________
[1] [Kate Norman Derr] “Mademoiselle Miss”: Letters from an American Girl Serving with the Rank of Lieutenant in a French Army Hospital at the Front, preface by Richard C. Cabot (Boston: Butterfield, 1916), 67.
[2] Helen Dore Boylston, Sister: The War Diary of a Nurse (NY: Ives Washburn, 1927), 237.
[3] Agnes Warner, ‘My Beloved Poilus’ (St. John: Barnes, 1917), loc 119,221, 324, 782.
[4] On the stench of gas gangrene, which suffused entire wards, see, for example, Edith Appleton, A Nurse at the Front: The First World War Diaries, ed. R. Cowen (London: Simon & Schuster UK, 2012), 194-95, 240: “One feels the horrible smell in one’s throat and nose all the time.”
[5] Shirley Millard, I Saw Them Die: Diary and Recollections (New Orleans, LA: Quid Pro, 2011), loc 1192. Even among gangrenous patients who survived, changing the dressings twice a day was an “agonizing procedure.” Beatrice Hopkinson, Nursing through Shot & Shell: A Great War Nurse’s Story, ed. Vivien Newman (South Yorkshire: Pen & Sword, 2014), loc 409.
[6] John & Caroline Stevens, eds., Unknown Warriors: The Letters of Kate Luard, RRC and Bar, Nursing Sister in France 1914-1918 (Stroud: History Press, 2014), loc 1790, 1704, 1713, 1722.
[7] Luard Letters, loc 306-315. Sadly, ‘the Prince of Wales’ died several days later.
[8] Derr, “Mademoiselle Miss, p. 47.
[9] Luard Letters, loc 2232.
[10] Derr, “Mademoiselle Miss,” pp. 95-96.
[11] Plus ça change, plus c’est la même chose. See Ann Jones’s graphic description of the work of army specialists in Mortuary Affairs who retrieve and bag body parts and liquefied innards of our fallen soldiers in Afghanistan. Ann Jones, They Were Soldiers: How the Wounded Return from America’s Wars – The Untold Story (Chicago: Haymarket, 2013), chapter 1 (“Secrets: The Dead”).
[12] Hopkinson, Nursing through Shot & Shell, loc 1442, 1498.
[13] Luard, Letters, loc 1273.
[14] Mary Borden, The Forbidden Zone (ed. H. Hutchison (London: Hesperus[1928] 2008), 83; Derr, “Mademoiselle Miss,”47; Luard Letters, loc 1767.
Copyright © 2017 by Paul E. Stepansky. All rights reserved. The author kindly requests that educators using his blog essays in their courses and seminars let him know via info[at]keynote-books.com.